UMaine-led team discovers protein, lipid connection that could help lead to new influenza therapies
Transcript
Sam Hess:
The big challenge is that people still get sick from the flu. The virus mutates every year, so the vaccine is playing catch‑up to that. We’d really like to have something that could fight the flu even though it’s changing, even though it’s mutating.
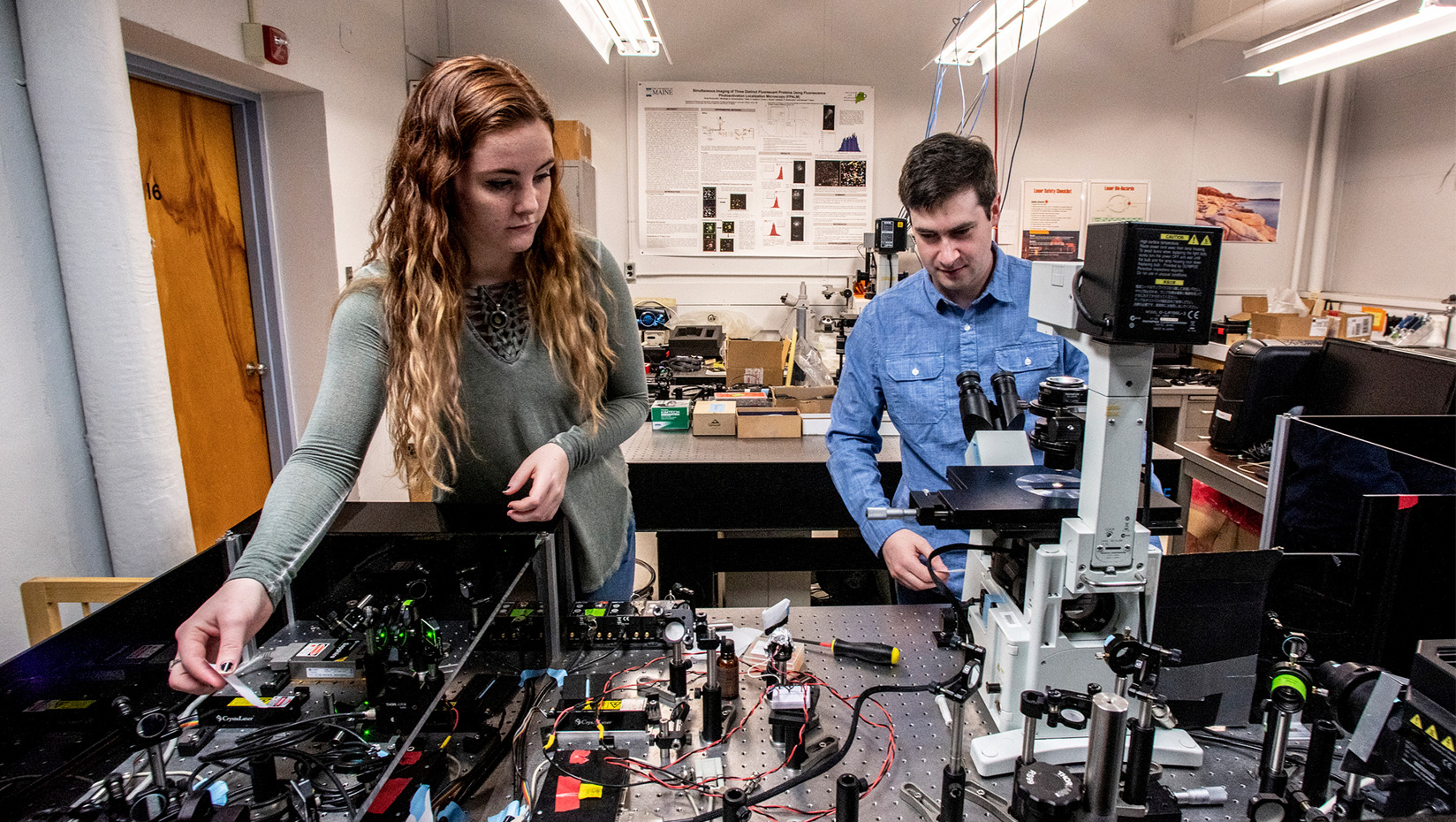
We’ve developed a technique called super‑resolution microscopy. It allows us to see what’s happening at the molecular scale, inside of a cell it’s either being infected by the flu or has some parts of the flu virus present. We discovered that one of the components, which is called HA or hemagglutinin, it’s the H in H1N1, is connected to a lipid that’s part of a host cell.
This lipid’s called PIP2. While many lipids are passive players, this particular one is able to signal or control signaling in the cell. That’s one thing that the virus could exploit. We discovered that the HA and the PIP2 are together in the same region and also that they affect each other, how they move, how they concentrate, and how they cluster.
That discovery means that there’s probably an interaction of some kind between these two things — the HA and the PIP2. If we could attack that interaction and break it up, then that could stop the virus from being able to manipulate the cell. We think that the HA and the PIP2 are interacting through the tail on the HA, which is a very short region. It’s very much consistent from strain to strain. I mean you could screen a bunch of different drugs to see if something is able to block that interaction.
This is a super‑resolution image of HA, the flu protein in green, and PIP2, which is the cell lipid. That’s colored in pink. There are areas where the two are together. It makes a strongly white cluster.
If you attack part of the virus that changes each year, then your strategy has to change as the virus changes. If you attack part of the virus that’s invariant, that’s conserved from year to year, and that’s what the tail is, it’s consistent, then either the virus gets killed by or isn’t able to replicate because of the drug, or the virus mutates something that it needs. Then it dies on its own.
It’s a connection that’s never been seen before. If we can block that interaction, then we have something that the virus can’t mutate out of. I think of this as like a bad relationship, three people that are competing. The HA is stealing PIP2 away from those other proteins, like a bizarre love triangle.
The target of vaccine and that’s …
I think it’s really exciting. Some people were quite surprised. I know some of my colleagues have heard what we found. They’re already planning some of the parts of their lab’s work to use this and investigate this finding further.
The flu causes tens of thousands of deaths per year in the United States. The available drugs for treating the flu are quite limited. The viruses that are circulating have resistance. Some of them have resistance to the available drugs.
All it takes is a few mutations to get us from the strains that are going around now into a 1918‑type flu. That type of virus would be a disaster. It was a disaster. We’d like to have some more options for fighting off something like that.
