Research Update: Diffuse Optical Imaging for Early Detection of Diabetic Polyneuropathy
by Liz Theriault, EPSCoR Student Writer
You may remember the days in elementary school where teachers would roll out a clunky projector and use transparent sheets, cameras, and light, to teach math, science, and more. What if there was a projector type machine that uses the same basic tools, but instead of teaching middle schoolers, it’s used for looking into the layers of your skin?
Karissa Tilbury, Assistant Professor of Chemical and Biomedical Engineering at the University of Maine has dedicated her time to developing low-cost biomedical optic techniques to expand accessibility for instrumental technology. Tilbury and her graduate student, Wyatt Austin, spent the summer of 2019 at the Biomedical Optic Technologies (BOT) Lab at Boston University under their awarded NSF RII Track-4 award (titled Diffuse Optical Imaging for Early Detection of Diabetic Polyneuropathy). NSF RII Track-4 awards provide opportunities for non-tenured investigators to further develop their individual research potential through extended collaborative visits to the nation’s premier private, governmental, or academic research centers.
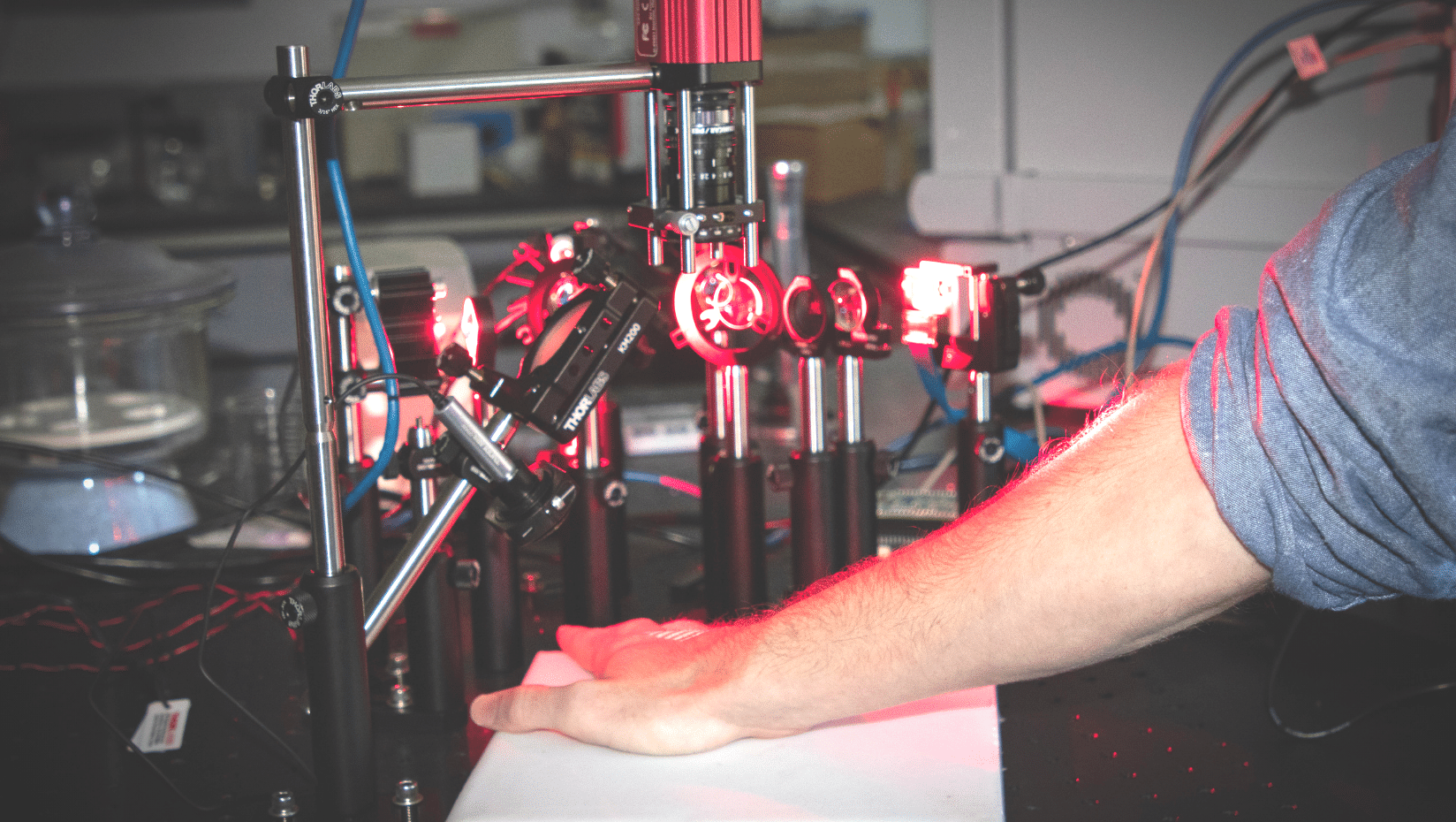
At the BOT Lab, the pair collaborated with researchers to build a spatial frequency domain imaging system (SFDI). This is where the resemblance to old-school projectors comes in. Essentially, an SFDI is composed of a number of LEDs, cameras, and projector screens that result in a noninvasive technique that allows users to peer into the different layers of skin.
“Multiple images at different wavelengths are captured and processed to extract tissue scattering and absorption properties which can be used to map oxy- and deoxyhemoglobin levels,” says Tilbury.
The practical approach of SFDI allows those who are at risk for or suffering from polyneuropathy, or damage to peripheral nerves in different areas of the body from diabetes, to take proactive detection measures.
“Current approaches for detecting neuropathy in diabetics use a tuning fork or a filament test, where a doctor applies a vibrating tuning fork or a filament to your skin and asks if you can feel it or not,” explained Tilbury. “That is very subjective, not very quantitative, and you can imagine that there is a lot of anxiety and doubt. But with [the SFDI] technique, we are upstream of current practices and can detect changes in different layers of the skin before it gets to the point where a patient cant’ feel the tuning fork.”
Working with collaborators at the BOT lab at Boston University allowed Tilbury and Austin to advance their understanding on SFDI technologies and bring it back to Maine, where an accessible SFDI machine could be vital for the older and more rural population.
“The reason SFDI is so powerful is that it is very low-cost. You could build a system for probably about $1,000 if you wanted to,” said Tilbury. “It’s attractable, it’s obtainable, and it’s a great educational tool and great for lower resource settings.”
Tilbury has plans to return to Boston University to finish out the NSF RII Track-4 award once COVID-19 related travel restrictions are lifted, with a tentative project end date of September 2021. Tilbury hopes to gain more advances in her research, while also gaining insights to smaller, day-to-day practices, such as organizational structures to lab meetings, that she can apply to her own lab at UMaine.
