Study discovers loss of innervation in fat related to obesity, diabetes, aging
To prevent conditions such as obesity and diabetes, as well as cardiovascular disease, researchers at the University of Maine are studying how the brain interacts with fat tissue.
“Our brain needs to communicate with fat tissue to burn calories, to increase our heat production, and to keep us metabolically healthy,” says Kristy Townsend, associate professor of neurobiology.
In a recently published study, members of Townsend’s lab discovered that in certain disease states, the nerves in fat tissue become neuropathic, or start dying.
Diabetic neuropathy already is known to happen in the skin, especially in the hands and feet, which leads to loss of sensation, as well as pain, numbness and tingling. However, the study is the first to show loss of proper innervation in fat beneath the skin, or subcutaneous adipose, under pathophysiological conditions such as obesity, diabetes and aging, according to Townsend.
The study, which was led by Magdalena Blaszkiewicz, formerly a Ph.D. student in UMaine’s Graduate School of Biomedical Science and Engineering (GSBSE) and now a postdoctoral researcher in the Townsend Lab, found that peripheral neuropathy is not restricted to classic tissues like the skin, and loss of innervation to adipose may trigger or exacerbate metabolic diseases.
The researchers found that as obesity levels went up, the amount of innervation in the fat went down.
“If we’re losing proper nerve supply and proper brain communication with our fat with a disease like diabetes, it’s probably getting worse because we can’t use those nerves to burn calories and keep ourselves healthy,” Townsend says, adding that obesity can lead to diabetes, so it’s important to keep fat tissue healthy in order to prevent this transition.
The researchers also demonstrated stimulation of adipose tissue neural plasticity with cold exposure, which could be a potential therapeutic option to promote nerve regrowth and restore metabolic health.
“One of the ways we know we can increase energy expenditure in the subcutaneous fat is through cold because it triggers thermogenesis, which causes heat and burns calories,” says Blaszkiewicz, who graduated from UMaine in 2019 with a doctoral degree in biomedical sciences. “What we didn’t know was whether or how that would affect nerve density in the adipose tissue.”
At the start of the project about five years ago, not many researchers were looking at nerves in the adipose tissue, according to Blaszkiewicz. The common idea, she says, was that there is a certain amount of nerves in the tissue that are static and don’t change.
“But what we saw with cold exposure was that the whole organ — the whole fat depot and the nerves within it — completely remodel, and there are areas where you have more innervation including in areas that previously didn’t have any,” she says.
The innervation increase could potentially lead to better metabolic health through the start of thermogenesis or lipolysis, the burning of stored fat fuels, Blaszkiewicz says.
Cold exposure also was found to increase the brain-derived neurotrophic factor, or BDNF, which maintains the nerves within a tissue and helps them survive and grow, according to Blaszkiewicz, who refers to it as “nerve food.”
However, cold exposure treatments offer several challenges. It can turn white fat into brown fat, which is thermogenic and healthy, but also requires burning a lot of calories, according to Townsend.
“We study energy balance, and we know that if you tip the scales and start burning more calories, you’re going to get hungry and want to take in more calories,” she says, adding that any cold exposure treatment or drug would have to be balanced with an appetite suppressant.
Another potentially harmful outcome would be negatively affecting other parts of the body such as the heart or bones, the researchers say, since activating the nerves that stimulate thermogenesis may do harm in these other tissues.
“Obesity is one of the most difficult diseases to treat because there are all these counter-regulatory things in our physiology that prevent us from losing weight,” Townsend says. “The key for us isn’t weight loss, but healthy metabolism no matter what your body weight is.”
Townsend says she and her team think the nerves in fat might play a role in staying healthy, including while aging.
“That’s important for Maine because we have the oldest median age in the country and lots of age-related diseases, and if some of those are due to loss of proper nerve communication to our tissues and organs, then we need to figure that out and see if there’s a way to mitigate it,” she says.
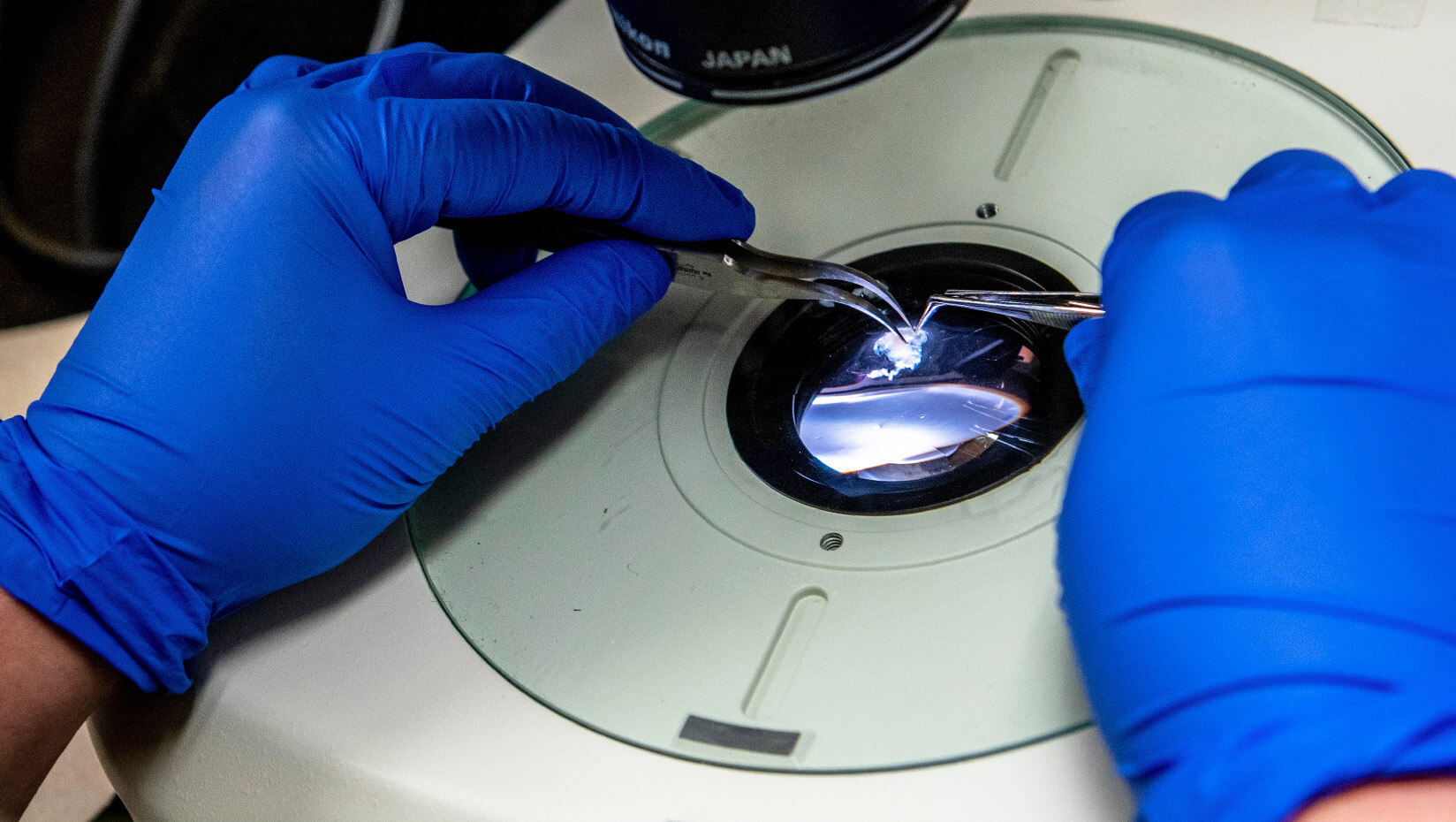
The study, which aligns with the University of Maine System “Research and Development Plan,” also looked at aging-related neuropathy and mapped out the entire adipose depot beneath the skin of a mouse, showing where the nerves were in the tissue.
“Neuropathy and neural plasticity in the subcutaneous white adipose depot,” was published in the journal PLOS ONE. It first appeared online as a preprint at bioRxiv. In addition to Blaszkiewicz and Townsend, co-authors include GSBSE collaborators Katherine Motyl of the Maine Medical Center Research Institute and Benjamin Harrison of University of New England, as well as seven undergraduate students.
“Part of our philosophy in our lab is that not only are undergrads involved in the research, but they contribute in such a way that they can be authors on papers. Our undergrads contributed really important data to the paper and they were part of discussions about what the data mean,” Townsend says.
Two of the students are now pursuing graduate degrees at UMaine.
Townsend’s lab is interested in how the brain and nervous system affect energy balance. A main goal is understanding what the nerves are doing in fat tissue and studying how those nerves play a role in keeping fat tissue healthy.
The next step for the researchers is looking at the neurotrophic factor that might be responsible for maintaining and regulating the remodeling of nerves in the adipose tissue.
“The goal for us now is figuring out the flavor of immune cells that release these healthy growth factors,” Townsend says. “Can we get those to travel into fat and make more growth factor and keep the tissue healthy?”
Blaszkiewicz is looking at how the immune cells move and change their identity to release the healthy growth factors.
Contact: Elyse Catalina, 207.581.3747, elyse.catalina@maine.edu
