Bioengineering students develop pediatric breathing simulator
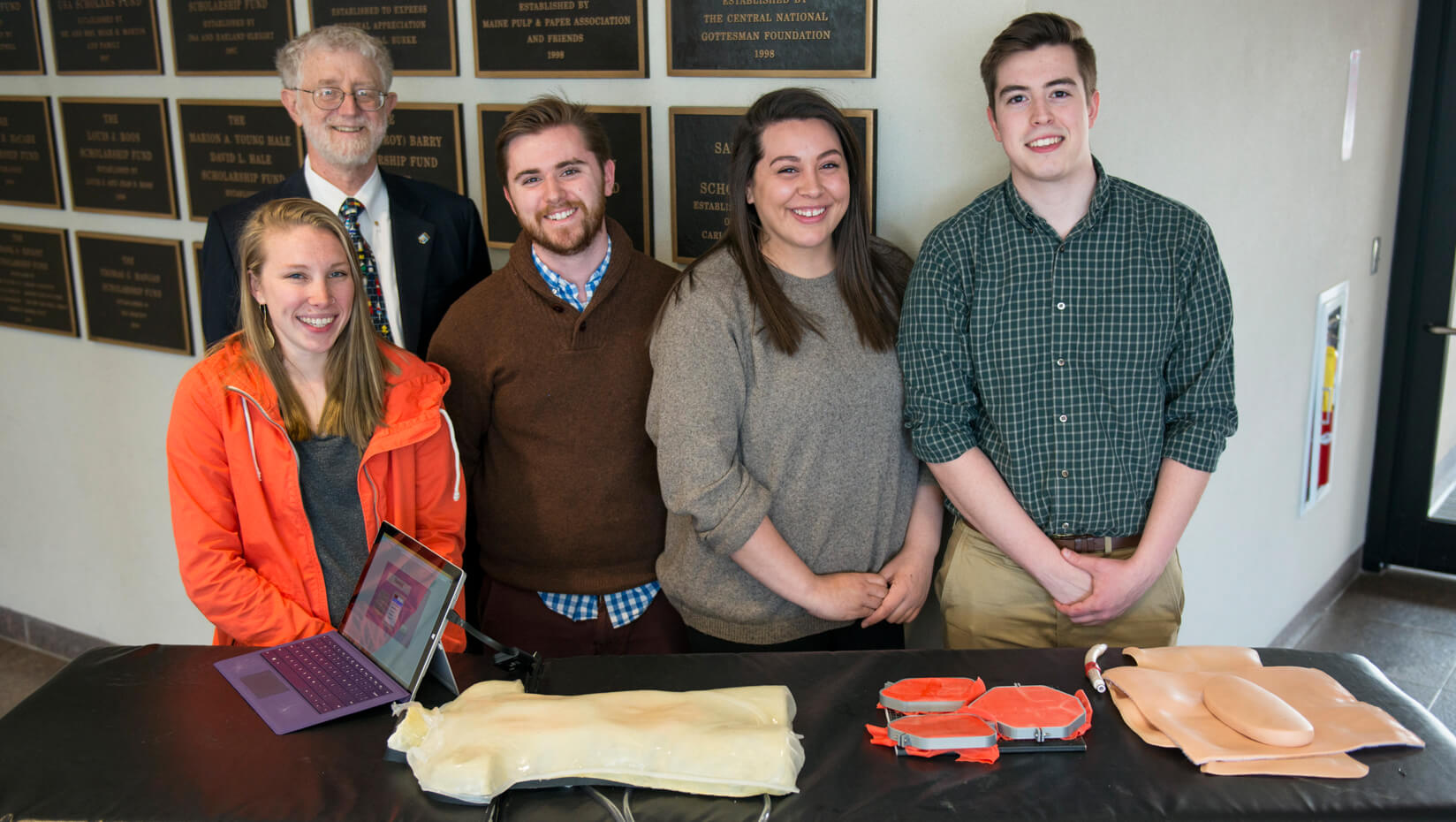
Four University of Maine bioengineering students have developed a new method of simulating pediatric respiratory distress in medical training manikins to better prepare health care professionals.
For their bioengineering senior capstone design project, the students were tasked with creating a pediatric breathing simulator capable of displaying realistic lung and diaphragm movements.
Most current manikins don’t have the ability to simulate lung and abdominal breathing independently, according to UMaine student Banton Heithoff, who worked on the project.
“Our manikin allows us to more accurately and realistically simulate breathing in children,” says Heithoff. “The big advantage of this manikin is that it allows us to more properly simulate critical conditions, so if a child is going into respiratory distress, they typically only use their diaphragm or abdominal breathing patterns, and in current manikins you can’t simulate this.”
Manikins designed to show different rates of breathing could potentially allow training doctors and nurses to make a diagnosis based on the breathing pattern, according to bioengineering professor Caitlin Howell, who advised Heithoff of Oldwick, New Jersey; William Patrick Breeding of East Granby, Connecticut; Amber Boutiette of Skowhegan, Maine; and Madeline Mazjanis of Portland, Maine.
Having more realistic training manikins can help health care professionals be better prepared for when emergencies occur, the students say. Current high-fidelity simulations for training doctors and nurses are expensive, and cheaper simulations are often not accurate, according to Howell.
The students were given a full-size training manikin by the UMaine School of Nursing to better understand how they are built. Using widely available materials — stretchable plastics, tubing, fittings and an air compressor — and a budget of about $500, the students designed a system that can accurately replicate four types of breathing patterns in the lungs and diaphragm.
Bioengineering majors are required to build a device during their senior year, and students usually work with clients from outside the university, Howell says.
For the project, the students worked in collaboration with Dr. Denham Ward and Dr. J. Randy Darby of the Hannaford Center for Safety, Innovation and Simulation (SIM) at Maine Medical Center in Portland, who acted as the clients. The students were advised by Howell and fellow bioengineering professor Karissa Tilbury.
Ward received a bachelor’s degree in electrical engineering from UMaine in 1969, and his professional career has spanned both the engineering and medical fields. Darby is a graduate of Knox College and the Tufts University School of Medicine, and directs the SIM Center. Ward and Darby worked with the UMaine College of Engineering and the students to develop the capstone design project.
“My research interest has always been respiratory physiology,” Ward says. “One of the things I’ve noticed on the simulation manikins is the breathing pattern is not very realistic, particularly in babies.”
Ward says babies have a soft chest wall, which allows for a lot of movement that is not simulated in most manikins.
In pediatric breathing simulations, Ward pointed out that training manikins only have lungs that fill and empty, but when children have trouble breathing, they use all their muscles and move their diaphragm, according to Howell.
“The right lung, left lung and abdomen don’t always breathe together,” Ward says. “If a baby aspirates a peanut in the right lung, then only the left side of the chest would be moving. We’d like a physician or a nurse to be able to recognize that when they saw a baby in the emergency room.”
Ward asked the students if they could create a manikin that would simulate the different breathing patterns. He gave the students specifications and offered feedback throughout the process.
“Dr. Ward was an invaluable resource because he works with the simulation manikins that are currently available,” Heithoff says. “By showing us what is currently available on the market and where those manikins are lacking allows us to see the holes we need to fill and also the standards we need to be at.”
The students are pursuing a patent for their prototype. Tilbury says she believes the design could be implemented into high-fidelity manikins to train nursing staff and future doctors, or even used in parenting classes that teach CPR.
“I didn’t realize we would actually be making a device that would be this realistic, useful and marketable,” Breeding says. “Everyone worked so well together that we were able to push out such a realistic device so quickly.”
The group presented their prototype April 24 at the UMaine Student Symposium at the Cross Insurance Center in Bangor.
Contact: Elyse Catalina, 207.581.3747
