Graduates of UMaine nursing program boost primary care in rural areas
In its first academic year, the Advanced Nursing Education Workforce program (ANEW) at the University of Maine supported 23 trainees and seven graduates who are providing care in rural, medically underserved communities across the state.
Recognizing the need for more family nurse practitioners (FNPs), UMaine’s School of Nursing launched the program in 2023 to financially support and educate students who are willing to work in areas with limited access to healthcare once they receive their degrees.
The Maine Center for Disease Control & Prevention states that Maine is considered the most rural state in the U.S. and that 40% of its population lives in one of 11 rural counties. The Health Resources and Services Administration (HRSA) designated each of the state’s 16 counties as Medically Underserved Populations. All but one — Cumberland, in which Portland is located — have been designated Health Professional Shortage Areas by the HRSA. Medically Underserved Populations and Health Professional Shortage Areas are identified using criteria such as population to health care provider ratios, poverty rates and percentages of adults 65 years or older.
To help bolster preventative and chronic disease care services for Mainers with limited access to health care, HRSA awarded UMaine a $1.9 million grant for 4 years to strengthen its FNP program. The grant’s focus is to produce nurse practitioners who will care for patients in rural, underserved areas, building on a dedication UMaine’s School of Nursing has held since 1992. Many ANEW graduates start working at primary care facilities designated as Federally Qualified Health Centers — nonprofit clinics that provide comprehensive care.
Haley Strout: Providing care for her rural community
Haley Strout graduated from the program in December 2023 and is working full time as a primary care provider at the Harrington Family Health Center, a Federally Qualified Health Center in Washington County. ANEW funded her final year in UMaine’s FNP program. A mother of three, Strout said her scholarship — totaling approximately $20,000 for the year — went above and beyond books and tuition.

“The biggest thing was the financial freedom that it really gave me,” Strout said. “I didn’t have to worry about picking up a side job to make tuition for that month. I was able to really just focus on studying and being prepared for my boards.”
ANEW scholarships can help with the student’s technology needs and costs associated with traveling to campus and clinical sites. Strout said it paid for her mileage and accounted for the wear on her vehicle from commuting two hours to UMaine from her home near Harrington.
She returned to UMaine to earn a graduate degree in nursing after her work as an EMT and emergency room nurse exposed her to rural communities’ challenge with accessing resources.
“In the ER, you see a lot of patients where maybe better access to primary care could have avoided their ER visit,” Strout said. “My interest started to shift at that point, from wanting the adrenaline of emergency medicine to being able to provide more one on one, education based care to my patients.”
“You see a lot of patients where maybe better access to primary care could have avoided their ER visit.”
Haley Strout
Family Nurse Practitioner,
Harrington Family Health Center
Strout said rural health concerns are the same as urban ones, but access to additional services and specialists create the difference. The Maine CDC lists barriers to transportation as a primary reason that adults over the age of 65 delay medical care. Rural area patients may have to drive an hour or more to see a specialist that is next door to someone living in Bangor or Ellsworth.
UMaine’s FNP program familiarized Strout with the resources she would have available working in a rural facility and also developed her relationship with a faculty member who she’s still able to utilize for guidance. Eva Quirion, a lecturer in the UMaine School of Nursing, is an active member of the Controlled Substance Stewardship program through the Schmidt Institute, which provides guidance on the use of controlled medications to clinics such as the one where Strout works.
“Something that my professor Eva said to me in my program was that you have to meet a patient right where they’re at, and that is different for every single patient,” Strout said. “It’s a lot of building trust, and it’s a lot of give and take, and it’s really understanding that addiction is a disease.”
Strout is easing herself into caring for patients with substance use disorder, something that she said is much needed throughout the state, especially in rural areas like Washington County where access to mental health resources is limited. Having grown up there, Strout said her familiarity with the people who live there have helped them be comfortable with her in return. Sometimes it is as simple as knowing how to tailor her explanations to patients in a way they’ll understand.
“You can’t do this job without having empathy for people,” Strout said. “You can’t do this job without constant self reflection and being open minded and just being dedicated to serving people.”
Susan Plissey: Bridging the gap in rural health care
Susan Plissey graduated from the FNP program in May 2024 and is working at the Katahdin Valley Health Center in Patten, a Federally Qualified Health Center. Plissey said working there helps her feel like she is able to reach patients who may have been turned away or received limited services at a traditional health care facility because of their ability to pay.
“I have always held a place in my heart for aging populations and underserved areas,” Plissey said. “You feel more impactful to those who have not always had access or felt heard in health care.”
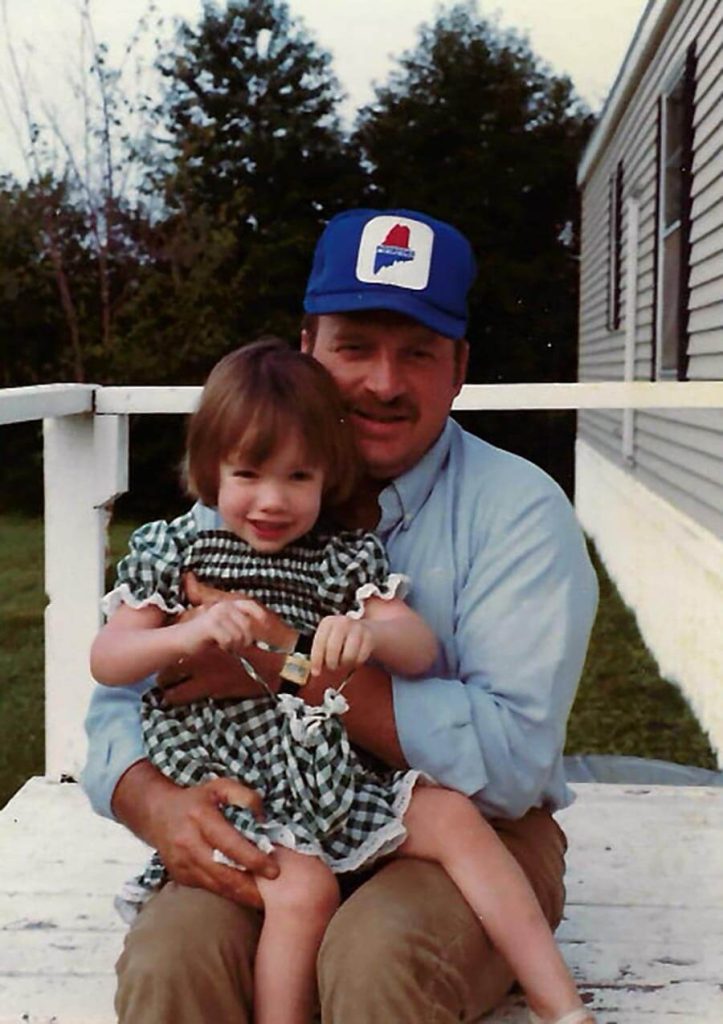
While her parents were raised on potato farms in Aroostook County, Plissey said they moved to southern New Hampshire with her when she was 4 years old and would come back to stay in the county during the summers. She moved to Fort Kent in 2006 and hasn’t looked back.
Without the ANEW grant, Plissey said she wouldn’t have been able to afford driving to the facility where she completed her clinicals, which is a 2-hour drive in each direction. In her last 2 years of the FNP program, she had to balance work, clinicals, education and childcare for her daughter, who was 5 years old by the time Plissey graduated.
It was also through the ANEW program that she connected with the only provider in a 4-hour radius who agreed to instruct her during her final semester of clinicals, which led to her current position as a provider in Patten.
Plissey worked as a registered nurse for 17 years before she returned to school for a graduate nursing degree. During those years, she said her exposure to rural families struggling to receive health care, either due to affordability or access to resources, encouraged her to become an access point for rural health care and bridge the gap of inequality between rural and urban settings.
“I was afraid that making the transition to being a provider might be uncomfortable or maybe even the wrong choice,” Plissey said. “However, I feel like I am making a positive difference in the community where I work, and that makes all the difference in satisfaction to me. I have time to look and listen to my patients without feeling time restraints or the pressure of quantity at the expense of quality.”
This Advanced Nursing Education Workforce (ANEW) Program is supported by the Health Resources and Services Administration (HRSA) of the U.S. Department of Health and Human Services as part of an award totaling $451,462 in year 2 with 0% financed with non-governmental sources. The contents are those of the author and do not necessarily represent the official views of, nor an endorsement, by HRSA, HHS or the U.S. Government.
Contact: Ashley Yates; ashley.depew@maine.edu